Paula Rochon, University of Toronto – Navigating Medication Awareness for a Healthier Tomorrow
 How many medications did you take today?
How many medications did you take today?
Paula Rochon, professor in the department of medicine and Dalla Lana School of Public Health at the University of Toronto, explains why it may be a few too many.
Dr. Rochon is Founding Director of Women’s Age Lab, a geriatrician and senior scientist at Women’s College Hospital and ICES. She received her medical degree from McMaster University and Master of Public Health from the Harvard School of Public Health. Dr. Rochon is a professor in the Department of Medicine at the University of Toronto (UofT) and is the inaugural RTOERO Chair in Geriatric Medicine at UofT. She is a Fellow of the Canadian Academy of Health Sciences and a Fellow of the Canadian Geriatrics Society
Dr. Rochon has a strong record of federal funding and has published more than 300 papers in peer-reviewed journals. She held the role of the Vice President of Research at Women’s College Hospital for 12 years. Dr. Rochon chairs the Canadian Institutes of Health Research (Canada’s federal funding agency) Institute of Aging Advisory Board to support research and promote healthy aging across Canada. She is the Deputy Editor of the Journal of the American Geriatrics Society).
Navigating Medication Awareness for a Healthier Tomorrow
Nearly 4 in 10 adults over the age of 65 living in the United States are prescribed five or more medications. Polypharmacy, the use of five or more medications, is prevalent among older adults, especially women managing chronic conditions. Although these medications are often important and necessary, they can come with risks like harmful side-effects, drug interactions and adherence challenges.
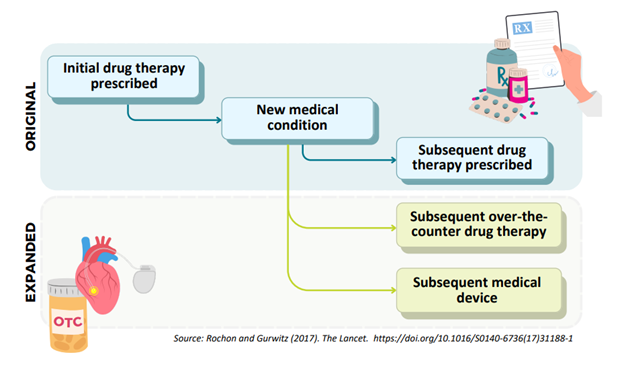
Imagine someone with knee pain is prescribed a nonsteroidal anti-inflammatory drug as a pain reliever, but that causes a subsequent side-effect of high blood pressure that is misinterpreted as a new medical condition; this leads to the prescribing of potentially inappropriate medication to treat the hypertension. When physicians mistake the side-effect of a medication for symptoms of a new medical condition, and prescribe a subsequent drug to treat it, it is known as initiating a “prescribing cascade.”
Prescribing cascades play an important role in polypharmacy. Recognizing these cascades is vital for healthcare providers to inform their medication reviews, and possibly, deprescribe medications.
Over 160 prescribing cascades have been identified, revealing how potentially inappropriate prescribing can be harmful. Women’s Age Lab’s most recent study emphasizes the impact of prescribing cascades on potential healthcare use.
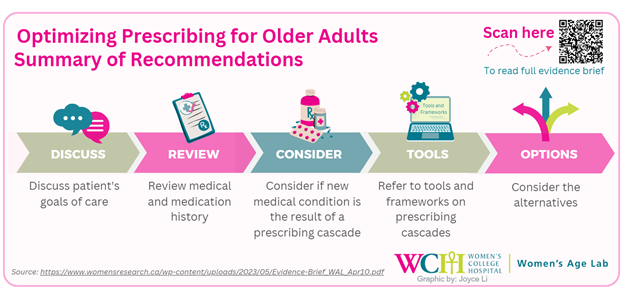
So, when a new medication is being considered or a patient’s medications are being reviewed, it is important to ask three questions:
1) Could an existing drug therapy be causing this new medical condition?
2) Could a lower dose be used or an alternative therapy initiated?
3) Is this drug needed at all?
By following these steps, potentially unnecessary medications can be reduced, side-effects can be mitigated and polypharmacy prevented.
Read More:
[The Lancet] – The prescribing cascade revisited
[Journal of the American Geriatrics Society] – Association of a calcium channel blocker and diuretic prescribing cascade with adverse events: A population-based cohort study


